Ambulance No Lights No Siren
Open Journal of Safe Science and Technology
Vol.iii No.3(2013), Commodity ID:37092,6 pages DOI:10.4236/ojsst.2013.33008
Predicting Use of Lights and Siren for Patient Illnesses
Western Transportation Institute, Montana State University, Bozeman, U.s.a.
Email: jessica.mueller@coe.montana.edu, laura.stanley@ie.montana.edu
Copyright © 2013 Jessica Mueller, Laura Stanley. This is an open admission article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original piece of work is properly cited.
Received May thirty, 2013; revised June 30, 2013; accustomed July xiv, 2013
Keywords: Ems; Lights and Siren; Emergency Manner; Transportation Rubber
ABSTRACT
Lights and siren are oft used by Emergency Medical Service (EMS) groups to reduce response times and increase a patient's take chances for survival. However, the utilize of lights and siren in EMS patient transport has been associated with occasional inappropriate utilise, college crash rates involving the ambulance, and a potential "wake outcome" increasing crash rates in ambient traffic. This study examines types of patient illnesses and their involvement with either emergency (lights and siren engaged) or non-emergency transport. Patient care records were analyzed from a five-year period from a private medical transportation company. A binary logistic regression model was congenital to predict the transportation manner (lights and siren or non-emergency-way) most probable to accompany each unique main patient illness. Patient illnesses were identified that showed a higher probability of transport using lights and siren. Fifteen illness descriptions were identified from the records as beingness more likely to result in emergency mode travel, including airway obstruction, contradistinct level of consciousness, animate problems, cardiac abort, cardiac symptoms, chest pain, congestive heart failure/pulmonary embolism, heart/cardiac, obstetrics, respiratory arrest, respiratory distress, stroke/cerebrovascular accident, trauma, unconscious, and patients where data was not entered. The patient illnesses associated with lights and siren were not limited to cardiac conditions and symptoms, which suggest that response-time goals based solely on cardiac arrest patients may demand to be expanded to include other illnesses such every bit respiratory weather condition. Expanded studies could assess whether or not lights and sirens result in a clinically meaning time savings across the spectrum of illnesses that are currently being transported using lights and siren. The list of illnesses identified hither every bit more than normally utilizing lights and siren could be useful to untrained European monetary system or dispatch workers to assist in minimizing unnecessary emergency manner travel, thereby increasing safety for Ems workers, patients, and the full general public.
1. Introduction
Standards regarding Emergency Medical Service (EMS) use of lights and siren in emergency medical ship have recommended that their employ in emergency medical vehicle (EMV) transport should be reserved for situations where improved response time will improve the patient'due south chance for survival or quality of life [1]. While using lights and siren during emergency response has been shown to meliorate response time, the use of lights and siren has besides been idea to cause an increased number of crashes involving vehicles virtually the ambulance [2]. The crash risk associated with this "wake effect" may outweigh the benefit associated with a slightly reduced response time. The goal of faster response time is to increase survivability in patients requiring time-critical medical attending. However, patient illnesses requiring timecritical response are relatively rare, and a limited list of illnesses has been examined in studies confirming increased survivability rates. The specific patient illnesses currently associated with EMV use of lights and siren deserve further report to determine whether the time saved in lights and siren travel is enough to justify their use in emergency response, or if the list of illnesses requiring lights and siren ship needs to be expanded.
1.1. Transportation Style in Ambulances
Calls for assistance from European monetary system care providers are divided into 3 main categories: emergency, urgent, and scheduled transports. An emergency ship involves a request for immediate assistance that requires utilise of lights and siren. An urgent transport is performed following a request for immediate assistance that does not require lights and sirens. Scheduled transports are previously arranged appointments to transport a patient, such every bit moving an elderly patient to a new care facility, that exercise not require utilise of lights or sirens.
ane.two. Transportation Style and Response Time
1 metric commonly used to evaluate EMS groups on their quality of provided care is the elapsed time from when a call is received until arrival on-scene. A new criterion that many EMS agencies are being encouraged by their managers to meet is a response time of eight minutes or less—a standard adult around a report of cardiac arrest patient outcomes in relation to response time [3]. Subsequent studies have not all agreed on the appropriateness of this eight-infinitesimal goal. Researchers supporting a reduction in response time take said that reducing this response time to v minutes would raise survival rates for cardiac arrest patients from 8 percent to ten pct [4]. By contrast, Pons and Markovchick [five] studied a grouping of nearly 3500 patients and plant no difference in survival rates whether response times were greater than or less than eight minutes.
Encouraging lower response times may atomic number 82 to Ems workers choosing to use lights and sirens in situations where the patient is stable. Lacher and Bausher [6] institute that EMS workers serving a pediatric hospital used lights and sirens inappropriately in near 40 percent of the calls in which lights and sirens were used. While the reasons for this were non identified, it was constitute that Ems workers with lower levels of training were more likely to appoint lights and sirens inappropriately than were more highly trained and certified paramedic personnel. Lacher and Bausher theorized this may be because the more than novice EMS workers were less comfortable with providing care en-road and wanted to discharge the patient to a facility that could provide more constructive care as quickly as possible. While the effect of inappropriate lights and sirens on crash rates is largely unknown, a study by Sanddal, Sanddal, Ward and Stanley [7] found a human relationship between increased crash rates and the employ of warning devices.
one.iii. Ambulance Crashes and Transportation Mode
Sanddal et al. studied ambulance crashes that occurred betwixt May 2007 and April 2009, identifying 409 dissever crashes from the European monetary system Network database. Of the ambulance crashes for which information was available well-nigh the use of warning devices (lights and/or sirens) at the time of the crash, 77 percent occurred while lights and/or sirens were in use. All of those crashes resulted in injury or death [7].
The majority of crashes resulting in injury occur while the ambulance is in an emergency state and with the injured parties unrestrained prior to the critical outcome [8,ix]. When an ambulance is involved in a collision, individuals in the rear of the vehicle (mostly EMS workers and patients) evidence higher fatality and injury rates than those driving or riding in the front [8]. The higher injury and fatality rate in the rear motel is related to the greater number of people in the rear of the motel besides as reduced rates of restraint utilize in the rear patient compartment.
The ambient traffic, or the vehicles that are traveling in proximity to the EMV, is also at take chances for crashes. A "wake event" has been described in which an EMV using lights and sirens causes other vehicles to collide without actual concrete involvement of the EMV. These crashes are difficult to runway, but Clawson et al. [2] plant potential wake-event crashes that numbered more than than v times the number of crashes that physically involved an EMV.
The patient intendance information collected in this report allowed researchers to perform analysis in an emergency transportation environs in social club to assess transportation modes used past European monetary system workers providing patient care in patient transports. The objective of this study was to highlight and explore any contributing furnishings that specific patient illnesses have on ambulance functioning in emergency mode. Agreement the relationship betwixt transportation fashion and patient condition could aid to influence standard accepted response times and to aid in training EMS workers or dispatch personnel near appropriate conditions for using lights and sirens during patient transports, potentially reducing EMS crash rates.
ii. Method
2.1. EMS Agency
The agency that provided records detailing patient care was the American Medical Response (AMR) ambulance service in Bozeman, Montana. Bozeman AMR is a paid, advanced life back up (ALS) emergency care provider, serving a population of nigh 100,000 people and responding to an average of 219 calls per calendar month.
2.2. Patient Care Records
Information used in this assay was collected from Patient Intendance Records (PCRs) provided by Bozeman AMR. A PCR is filled out as part of standard protocol for every patient send, and its contents detail specific information pertaining to patient illness and medic responsive activities while under the intendance of an EMS worker. Institutional Review Board approving was granted for this study, and all data provided by AMR Bozeman was censored to eliminate any identifying patient or location information. The record set used for analysis includes all PCRs submitted by AMR between July 2, 2005, and July 1, 2010. This data set represents 13,253 private calls. Tabular array 1 shows a pick of relevant fields from those records along with a description and examples of data entry values from the PCRs.
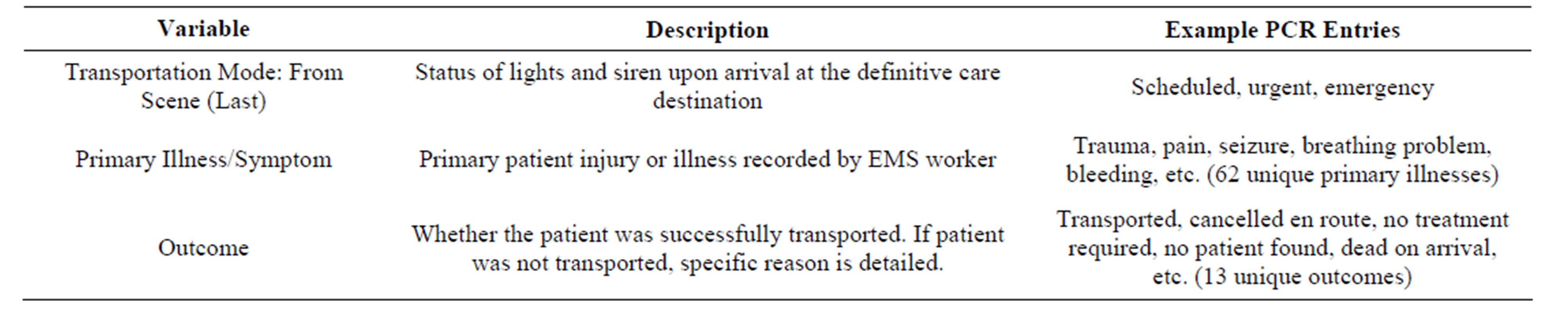
Table 1. Patient care record variable descriptions.
Transportation Mode is a categorical variable, indicating the emergency status of the ambulance during travel. Primary patient affliction is the primary injury that resulted in the need for EMS care or transportation. Each patient send is associated with only one main illness.
2.3. Data Reduction
Of the xiii,253 PCRs examined, the merely records included in this analysis were those with an outcome of "Transported," which excluded 3802 records. Excluded patient outcomes include "Patient Refused AMA" (2345 records excluded), "Cancelled FD/PD" (702), "Cancelled ENR" (386), "Dead On Inflow" (97), "No Patient Institute" (84), "No Treatment Req'd" (53), "Elevator Assist" (48), "InterFacility" (29), "Treated and Pronounced" (26), "Law Custody" (17), "Treat/No Trans". (14), and "Helicopter" (1). Other records excluded were those in which the main illness department of the form was not filled out (76 records excluded).
Data were adjusted to more specifically define transportation mode. As shown in Tabular array i, in that location are three outcomes for transportation mode: scheduled, urgent, and emergency. This analysis treated transportation mode equally a binary variable (emergency/non-emergency), combining scheduled and urgent calls as "non-emergency" trips where lights and siren were non used.
2.4. Data Analysis
Initially an inflated binary logistic regression model was built including all levels of patient affliction equally predictor variables. A definitive model could not be built due to quasi-complete separation of information. This was evident in the information for the patient affliction "Nausea". There were 229 instances where nausea was the primary patient disease, but in that location were zero instances where nausea was the primary patient illness while the ambulance traveled in emergency transportation way.
The Proc Logistic process was applied in SAS (version 9.iii) to build a binary logistic regression model using the remaining variables to predict the binary response (emergency transportation manner vs. non-emergency transportation manner).
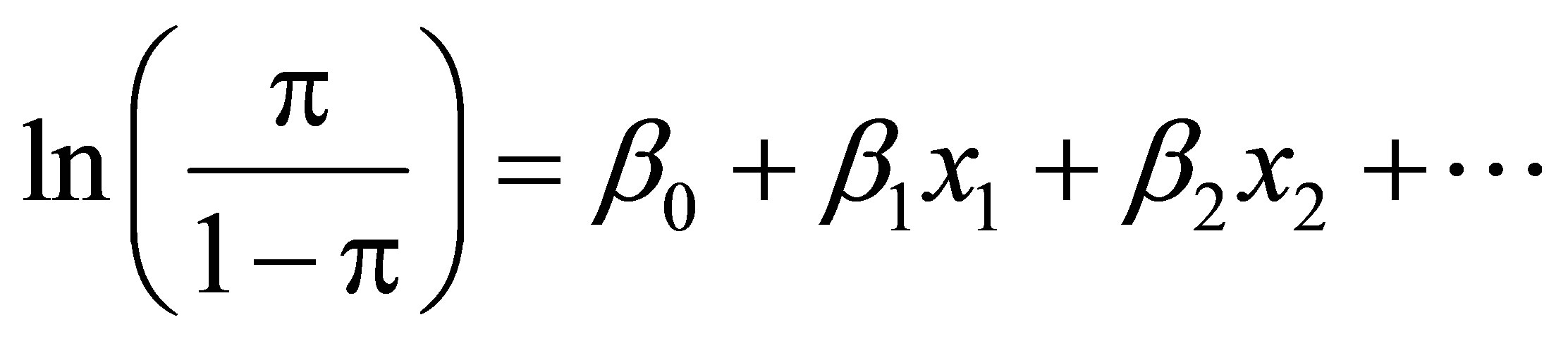 (1)
(1)
where:
π represents the probability of experiencing emergency transportation mode;
 is referred to as the odds ratio;
is referred to as the odds ratio;
 is a parametric change in the odds ratio associated with a the presence or absence of the predictor i, such that
is a parametric change in the odds ratio associated with a the presence or absence of the predictor i, such that  is the modify in odds of an occurrence associated with the presence of that predictor [ten];
is the modify in odds of an occurrence associated with the presence of that predictor [ten];
xi is the presence or absence of the predictor i.
Significant predictors are reported along with their odds ratios and confidence intervals on those odds ratios. Patient illnesses that were non evaluated in the regression model due to separation of data and under-represented events were analyzed separately to determine if each response was overrepresented in emergency or not-emergency transports. Because the contingency table cells take both very small-scale (event) and very large (non-issue) values, neither Chi-Foursquare nor Fishers' Exact Test was possible, just the percent association is reported.
iii. Results
Master Patient Illnesses Contributing to Emergency Mode
All patient illnesses that had zero events in either emergency or non-emergency mode were dropped from the model. Dropped illnesses include shock (1 observation), "Behav/Psych" (229), "Nausea" (126), "Vertigo" (54), "Fever/Influenza" (44), "CP-Musc/Skeletal" (35), "Epistaxis" (xx), "Hypertension" (xx), "Dehydration" (xviii), "Diarrhea" (18), "Swelling" (16), "Hypothermia" (14), "Eye Trouble" (12), "Malaise" (eight), "Ecology Injury"(4), "Mass/Lesion" (3), "Newborn"(3), "Contagious Affliction" (one), "Device/Equip Prob". (one), "Drainage/Discharge" (one), and "Not App". (10). Shock was but observed during emergency transportation mode, and the remaining dropped patient illnesses were observed only during nonemergency transportation mode.
The patient illnesses that were establish to exist significantly higher odds of existence transported using lights and siren included airway obstruction (odds ratio: five.7 times more probable to use lights and siren), altered level of consciousness (2.3), breathing bug (two.three), cardiac abort (262.iii), cardiac symptoms (4.0), breast pain (2.9), congestive middle failure/pulmonary embolism (9.two), heart/cardiac illness (nine.8), condition not entered on paperwork (iii.1), obstetric conditions (7.4), respiratory arrest (66.4), respiratory distress (5.4), stroke/cerebrovascular accident (3.eight), trauma (2.8), and unconscious patient or unknown status (sixteen.0). Figure 1 should be interpreted equally follows: a transport with a patient whose master affliction is "Airway Obstruction" increases the likelihood of emergency transportation over non-emergency transportation mode by 100.75, or five.7 times.
four. Discussion
Identifying patient illnesses that increment the likelihood of emergency fashion transport tin can be helpful to EMS workers who may not have the experience or ability to quickly assess patient status or whether that condition requires the use of lights and siren during ship. Illnesses that were found to be associated with higher likelihood of transportation using lights and sirens include: airway obstacle, contradistinct level of consciousness (LOC), breathing problems, cardiac illnesses, respiratory illnesses, stroke, trauma, chest pain, obstetric illness (OB), and congestive heart failure or pulmonary embolism (CHF/ PE). This information is largely known or suspected by the European monetary system community, but this analysis considerately substantiates that cognition.
While lights and siren can be used to reduce the time transporting a patient to definitive intendance, the interval of fourth dimension between the initial telephone call for aid and the ambulance arriving on-scene is as well important. The list of critical illnesses generated in this written report tin can too be of utilize to dispatch personnel who inform responding Ems workers about the condition of the patient prior to their arrival on the scene. For example, if a patient requested help with a master complaint of nausea (0 of 226 patient transports due to nausea used lights and siren), the dispatch personnel could laissez passer the data on to the responding EMV so they could travel to the patient without using lights and siren. An EMS dispatch coding system is already in use; however, there is some discrepancy in how dispatch personnel classify patient status and severity compared to on-scene responding EMS workers. Neely et al. [11] studied whether Ems acceleration codes were equivalent between dispatch and the responding paramedic and establish a trend of dispatcher "overcoding", where the acceleration-assigned code was more severe than the code assigned by the paramedic. It was unclear whether this overcoding was due to excessive dispatcher circumspection or existing protocol. The trend that Neely observed may have also been evident in our transportation data— while but five.4 percent of patient transports from the scene to definitive care used lights and siren, almost 87.4 percent of the travel en route to the patient was conducted in emergency mode. However, we cannot attribute this discrepancy to dispatch code consignment; our data set does not include the specific dispatch codes, only the mode of transportation that could have been chosen past EMS workers independently of acceleration data. An objectively generated list of illnesses requiring urgent response may be of use to help dispatch perform more accurate assessments about the urgency required in requests
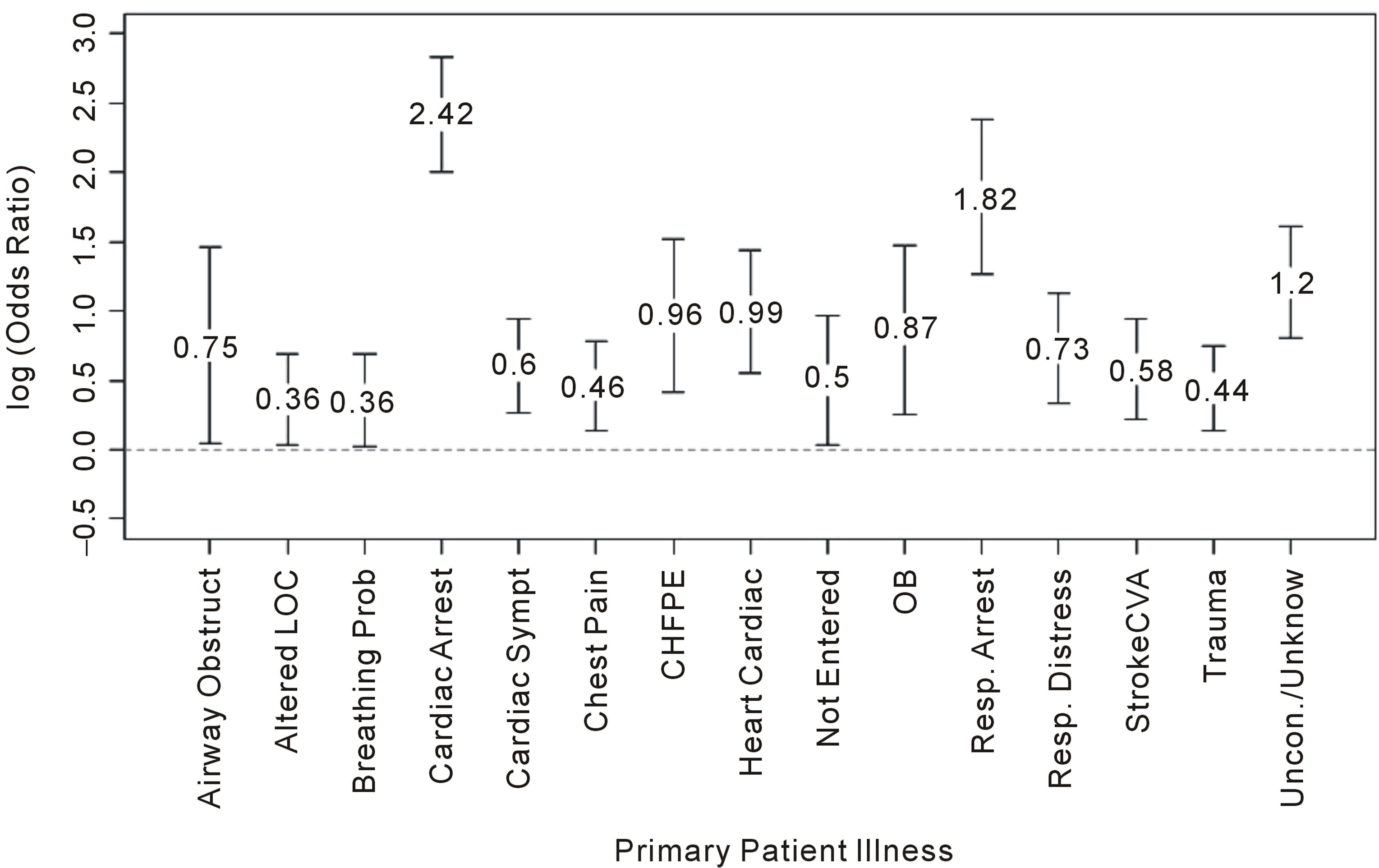
Figure 1. Log odds ratios and 95% CIs for association of patient illnesses with lights and siren.
for EMS response, thus minimizing the number of Ems responses using lights and siren. Additionally, patient illnesses that may not require immediate medical attention tin be referred to medical advice hotlines or alternative Ems services in order to keep Ems resources bachelor to respond to more than critical patients.
A study by Maio et al. [12] that examined data from European monetary system transports nerveless survey responses from experts detailing several aspects of patient outcome, including a "survival" metric for different illnesses. An interesting extension to Maio's report could exist an examination of high "survival" scores (indicating illnesses where the bear on and relevance of survival is important) and their relationship with frequency of transport using lights and siren. Results from such an assay could identify illnesses that practise non have an bear on on patient survivability just that commonly lead to transports using lights and siren.
The purpose of using lights and siren during response and patient transportis to reduce emergency call response times. Nonetheless, the time saved past using lights and siren may not exist clinically significant. Studies that take compared EMV response times for emergency and not-emergency transport accept constitute time savings as small every bit 43.5 seconds [13]. A more contempo study constitute a larger fourth dimension savings of two.62 minutes [fourteen]; however, this was non constitute to amend patient outcomes where patient care was administered in the ambulance. The current eight-minute goal for response time exists because of a study that focused specifically on cardiac arrest patients and their outcomes in relation to transportation fourth dimension [three]. The list of patient illnesses enumerated in our study contains more than than cardiac abort and related symptoms. Further enquiry should be performed to come across if European monetary system response to these additional illnesses is being conducted with the advisable warning measures (lights and siren when patient is non stable), or if the standard for response time should be adjusted to business relationship for the time-disquisitional responses needed for the additional patient illnesses.
1 studied phenomenon associated with emergency manner is the existence of wake effects, which draw the higher charge per unit of crashes among nearby vehicles that appears to be caused by the emergency vehicle operating with lights and sirens [ii]. While the causes of this wake effect have not been explicitly identified, it is hypothesized that the crashes are due to the emergency vehicle's lights and sirens affecting the actions of drivers in surrounding vehicles. With proper training, knowing which patient illnesses require lights and sirens could help EMV operators minimize the time spent operating in emergency mode inappropriately, potentially limiting wake effect crashes. Analysis of trends describing which patient illnesses are generally associated with emergency mode could help to identify potential "offending" illnesses—that is, illnesses that are idea to require emergency response but for which emergency response does not actually affect the patient survivability rate. Preparation could be particularly beneficial for novice EMS workers, who may tend to inappropriately engage lights and siren [6] considering they are not comfortable deciding which illnesses explicitly warrant the use of lights and sirens during transport.
4.1. Hereafter Studies
Another application of these findings would be for researchers to compare the interactions of the EMS agency studied here with European monetary system groups in different population and geographical areas. Collecting the data used in this analysis required minimal attempt, as it is already kept in electronic formats for billing and legal purposes past the Ems agencies.
4.2. Limitations
The data analyzed in this study were from a single European monetary system care provider, and and then inference cannot be made to a broader patient grouping than that found in Bozeman, Montana, every bit the distribution of patient illnesses and injuries seen in this study may be specific to AMR Bozeman's service surface area. Nevertheless, the data used in this study are typically maintained by most major healthcare providers for billing purposes, so other agencies should be able to reproduce the analysis quickly. Information on dispatch codes was unavailable for written report. Without this information, assay was non able to be conducted regarding the agreement of emergency or non-emergency coding betwixt the European monetary system workers and dispatch. The data were gathered from paperwork filled out by EMS workers during and later on patient transportation, so it is possible that there are some paperwork errors or omitted data points. Finally, because information describing specific EMS worker training level was not bachelor, cess of the effect of Ems preparation level on whether or not transports used lights and siren was not possible.
5. Conclusion
This report presents a list of illnesses that frequently result in patient transports using lights and siren. While previous studies focus mainly on cardiac injuries, these findings suggest that survivability studies related to transport time and fashion of transportation should be expanded to include respiratory illnesses. The list of illnesses highlighted here will additionally exist helpful in training novice EMS workers or dispatch personnel who may lack the expertise or conviction to accordingly and speedily appraise patient condition, resulting in less frequent travel with lights and siren, thereby increasing transportation safety.
REFERENCES
- National Association of Emergency Medical Services Physicians [NAEMSP], "Utilise of Warning Lights and Siren in Emergency Medical Vehicle Response and Patient Transport," Prehospital and Disaster Medicine, Vol. nine, No. 2, 1994, pp. 133-135.
- J. Clawson, R. Martin, 1000. Cady and R. Maio, "The Wake Effect: Emergency Vehicle-Related Collisions," Prehospital and Disaster Medicine, Vol. 12, No. 4, 1997, pp. 274- 277.
- Pre-Hospital Trauma Life Back up Commission of the National Association of Emergency Technicians in Cooperation with the Committee on Trauma of the American College of Surgery, "PHTLSC—Basic and Advanced Pre-Hospital Trauma Life Support," 3rd Edition, Mosby, New York, 1998.
- J. P. Pell, J. Thou. Sirel, A. K. Marsden, I. Ford and S. M. Cobbe, "Issue of Reducing Ambulance Response Times on Deaths from out of Hospital Cardiac Arrest: Cohort Written report," British Medical Journal, Vol. 322, No. 7299, 2001, pp. 1385-1322. doi:10.1136/bmj.322.7299.1385
- P. T. Pons and V. J. Markovchick, "Eight Minutes or Less: Does the Ambulance Response Time Guideline Impact Trauma Patient Outcome?" The Journal of Emergency Medicine, Vol. 23, No. 1, 2002, pp. 43-48. doi:10.1016/S0736-4679(02)00460-two
- M. E. Lacher and J. C. Bausher, "Lights and Sirens in Pediatric 911 Ambulance Transports: Are They Being Misused?" Annals of Emergency Medicine, Vol. 29, No. 2, 1996, pp. 223-227. doi:10.1016/S0196-0644(97)70272-v
- T. 50. Sanddal, Northward. D. Sanddal, Northward. Ward and L. Stanley, "Ambulance Crash Characteristics in the United states Defined by the Popular Press: Aretrospective Analysis," Emergency Medicine International, Vol. 2010, No. 2010, 2010, pp. one-7. doi:10.1155/2010/525979
- L. R. Becker, E. Zaloshnja, Northward. Levick, G. Li and T. R. Miller, "Relative Risk of Injury and Death in Ambulances and Other Emergency Vehicles," Blow Assay & Prevention, Vol. 35, No. 6, 2003, pp. 941-948. doi:10.1016/S0001-4575(02)00102-i
- C. Kahn, R. Pirrallo and East. Kuhn, "Characteristics of Fatal Ambulance Crashes in the United States: An 11-Twelvemonth Retrospective Analysis," Prehospital Emergency Care, Vol. 5, No. 3, 2001, pp. 261-269. doi:10.1080/10903120190939751
- A. Agresti, "An Introduction to Chiselled Data Analysis," 2d Edition, John Wiley and Sons, Inc., Hoboken, 2007. doi:x.1002/0470114754
- K. West. Neely, J. A. Eldurkar and M. East. R. Drake, "Practice Emergency Medical Services Acceleration Nature and Severity Codes Concord with Paramedic Field Findings?" Bookish Emergency Medicine, Vol. 7, No. 2, 1999, pp. 174-180. doi:10.1111/j.1553-2712.2000.tb00523.x
- R. F. Maio, H. G. Garrison, D. W. Spaite, J. S. Desmond, M. A. Gregor, C. K. Cayten and I. M. Stiell, "Emergency Medical Services Outcomes Project I (EMSOP I): Prioritizing Conditions for Outcomes Research," Annals of Emergency Medicine, Vol. 33, No. 4, 1999, pp. 423-432. doi:ten.1016/S0196-0644(99)70307-0
- R. Hunt, Fifty. Brown, Eastward. Cabinum, T. Whitley, N. Prasad, C. Owens and C. Mayo, "Is Ambulance Transport Time with Lights and Sirens Faster than That Without?" Annals of Emergency Medicine, Vol. 24, No. 4, 1994, pp. 507-511.
- A. Marques-Baptista, P. Ohman-Strickland, K. Baldino, M. Prasto and 1000. Merlin, "Utilization of Alarm Lights and Siren Based on Hospital Time-Critical Interventions," Prehospital and Disaster Medicine, Vol. 25, No. 4, 2010, pp. 335-339.
Abbreviations
EMS: Emergency Medical Service EMV: Emergency Medical Vehicle ALS: Advanced Life Back up PCR: Patient Care Record LOC: Level of Consciousness OB: Obstetric CHF/PE: Congestive Middle Failure or Pulmonary Embolism
Ambulance No Lights No Siren,
Source: https://www.scirp.org/html/4-1480069_37092.htm
Posted by: pettyhattlem88.blogspot.com


0 Response to "Ambulance No Lights No Siren"
Post a Comment